- Author
- Date
- 2025-12-26
- Views
- 119
You did everything right. You wore sunscreen. You switched creams. You avoided the sun passionately with a skincare routine. And yet, those brown patches on your cheeks, forehead, or upper lip are still sitting there…smugly.
Welcome to melasma: the skin condition that refuses to take a hint. Melasma is often mistaken for a simple tan or leftover marks from acne, but it is far more complex than that. It is a chronic pigmentation condition in which the skin produces excess melanin in response to multiple triggers, most commonly sunlight, hormonal changes, and genetic predisposition.
Because these triggers are ongoing and challenging to avoid altogether, melasma tends to persist and may return even after treatment. This is what makes it particularly frustrating for many people.
What exactly is melasma?
Melasma is a chronic pigmentary disorder characterized by brown to grey-brown patches, usually on sun-exposed areas of the face: cheeks, forehead, nose, chin, and that notorious area above the upper lip.
It occurs when melanocytes, the pigment-producing cells, go into overdrive and start depositing excess melanin in the skin, sometimes in the surface layers, sometimes deeper, and often both. And here’s the most important part: It isn’t just a skin issue. It’s a skin + hormone + sun + genetics + inflammation problem rolled into one. No wonder, it’s a stubborn condition!
|
Melasma at a glance
|
Why does melasma happen?
Melasma doesn’t show up because you “did something wrong with your skincare routine.” It shows up because several triggers come into play at once.
✔ Is sunlight the main villain?
Ultraviolet (UV) rays and even visible light stimulate melanocytes. That’s why melasma often worsens in summer and slightly improves in winter. One unprotected exposure to the sun can undo weeks of treatment. It may sound dramatic, but it is true.
✔ Hormones: The invisible instigators
Melasma is linked with:
- Pregnancy—‘Mask of Pregnancy’
- Oral contraceptive pills
- Hormonal therapies
- Thyroid disorders (in some people)
Hormones don’t just increase pigment; they make melanocytes more sensitive to light. So, even minimal sun exposure can trigger pigmentation.
✔ Genetics: family matters
If anyone in your close family had melasma, your skin may already be primed for it. Genetics influence how reactive your melanocytes are, and how deeply pigment gets deposited.
✔ Inflammation & skin irritation
Harsh scrubs, aggressive facials, inappropriate lasers, or overuse of “brightening” products can inflame the skin. Inflammation tells melanocytes to produce more pigment.
Alert: Trying too hard to fix melasma can actually make it worse. Follow your dermatologist’s prescriptions and instructions.
Why melasma refuses to fade
Melasma treatment remains challenging. Melasma management is also important due to inconsistent results and frequent recurrences. It also targets the facial region, leaving a detrimental influence on patients’ overall well-being and directly damaging their psychological and emotional state. This is where many patients feel defeated.
Melasma behaves like a chronic condition, similar to asthma or diabetes. You can control it; but not cure it forever. The main reasons for which melasma keeps coming back are:
- 1. Pigment may be deep in the dermis, not just on the surface.
- 2. Melanocytes remain hyper-responsive.
- 3. Triggers (sun, heat, hormones) never entirely disappear.
- 4. Treatments fade pigment but don’t “reset” melanocytes.
Types of melasma: Why it’s important to get it diagnosed correctly
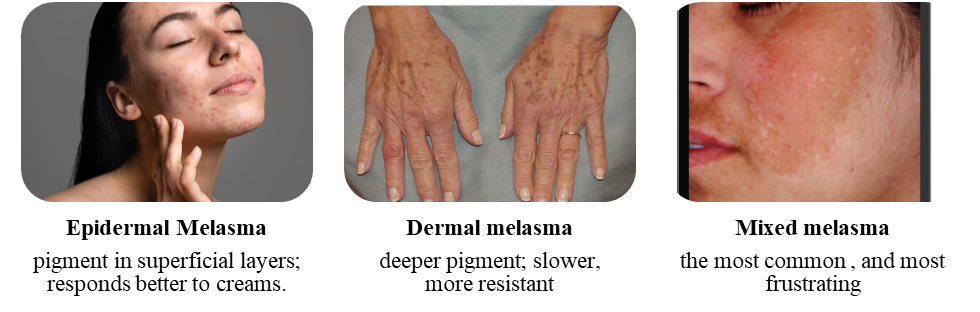
Not all melasma is same, and treatment success depends on the site of the pigment. A dermatologist may use a Wood’s lamp, dermoscopy, or clinical judgement to assess this. The most crucial point in melasma is not to self-diagnose yourself with Google!
What actually helps?
Melasma treatment is an ongoing process and will not give instant or overnight results. But with the right strategy, it can be controlled.
1) Sun protection: non-negotiable
This is the backbone for everything.
- Broad-spectrum sunscreen (SPF 30-50+)
- Preferably tinted sunscreens (they block visible light too)
- Reapply every 2-3 hours if outdoors
- Hats, scarves, umbrellas = very important, though underrated
Please note: no sunscreens = no progress.
2) Topical treatments
Commonly prescribed treatments include: Hydroquinone (gold standard, however, needs supervision), Azelaic acid, Kojic acid, Tranexamic acid, Retinoids, and Niacinamide. Please seek your dermatologist’s advice before using any topical treatments.
Important rule: More Products ≠ Better Results
Overuse = Irritation = Darker Melasma.
3) Oral treatments
Oral tranexamic acid, antioxidants, or supplements may help some patients, but only under medical guidance. This is not a DIY zone.
4) Procedures: proceed with caution
Chemical peels, lasers, and energy-based devices can help, but they can also backfire if done incorrectly. Melasma-friendly procedures require correct patient selection, conservative settings, and strict sun avoidance afterward. Aggressive lasers + melasma = regret.
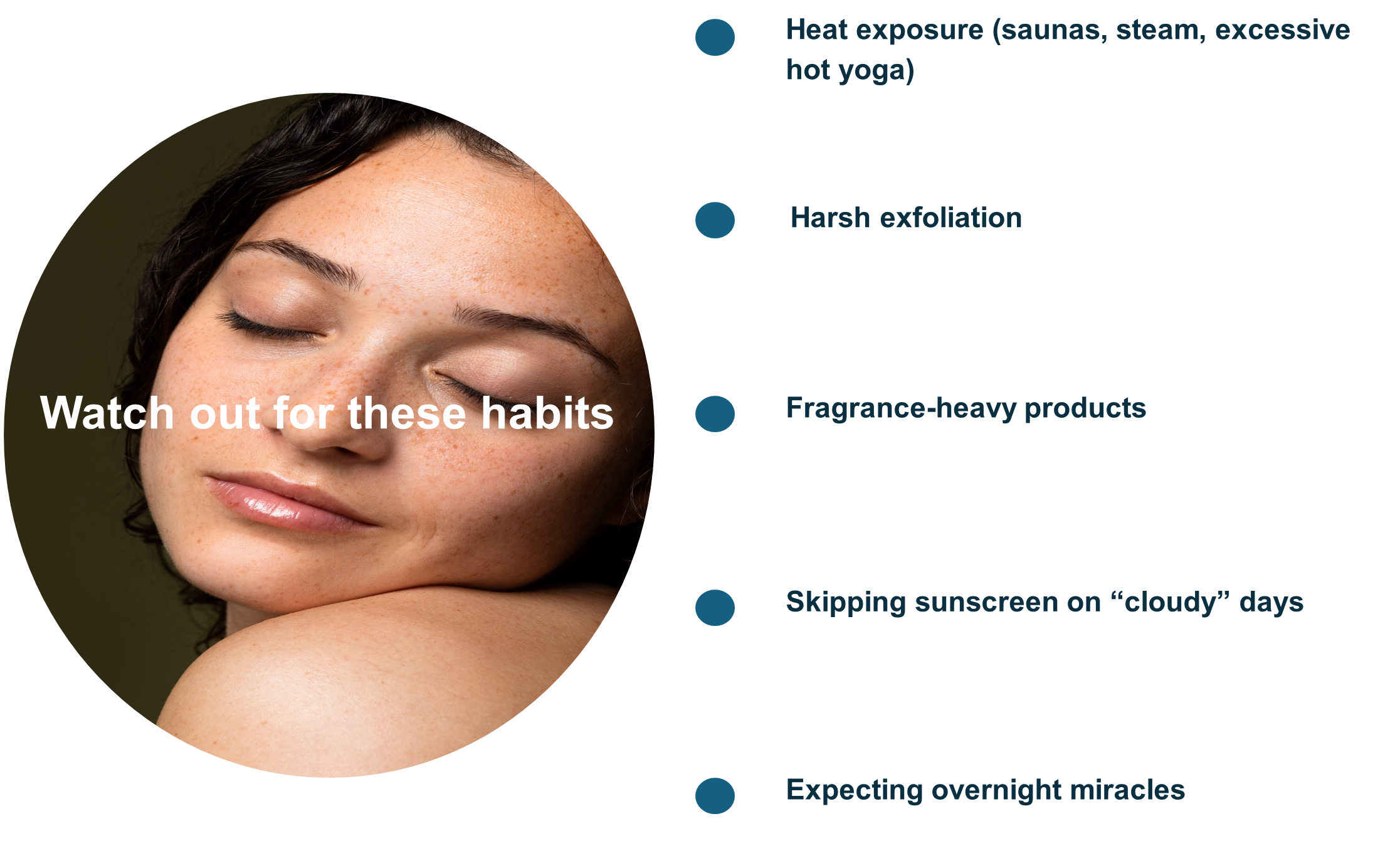
Skincare habits that quietly sabotage progress: Melasma responds best to consistency, not intensity.
The emotional side of melasma
Melasma doesn’t hurt, but it has lasting effects on confidence. Many patients report feeling older than they are, avoiding photos or social events, constantly covering up with makeup, and being told to “just ignore it!”
Your frustration is valid. Melasma affects quality of life, not just appearance, and recognizing that is a critical aspect of management.
The bottom line...will it ever go away?
Melasma can fade significantly, remain well-controlled, and even become barely noticeable, however, it requires:
- Long-term management, so plan patiently and think long-term
- Avoid any triggers that may exacerbate the condition
- Ongoing maintenance treatment
- Realistic expectations
Think control, not cure.
One of the most important things is to stop blaming yourself and start working with your skin instead of against it. This is the beginning of improvement!
Remember: Melasma isn’t stubborn because you’re careless. It is stubborn because it’s biologically wired to be. With the proper guidance, patience, and protection, you can keep it in check. Melasma may be persistent, but so are you!
References:
1: Wang LJ, Pang YB, Li WQ, et al. Front. Pharmacol. 2024; 15. DOI: 10.3389/fphar.2024.1421499.
2: Majid I, Aleem S. Journal of skin and stem cell. 2022; 8: 4. DOI: 10.5812/jssc.120283.